Diana Rahima – Sukaina Mahdi – Luay Ruhaibani – Saleh Malas
“I was 15 when my chronic depression started. In an attempt to distract myself from it, I would study, or even feign forgetfulness. I tried not to stay focused on the symptoms.”
Zeina, whose last name is withheld at her request, did not turn to a specialist or a psychiatrist when her psychological state deteriorated, but rather she spoke to teachers, who helped her feel better briefly.
Zeina turned 31 this year. She told Enab Baladi about her hesitation to see a psychiatrist for consultancy. Doing so was not the best idea where she lived in the city of Aleppo, northern Syria. Since a psychiatrist is considered a “doctor for crazy people,” she did not disclose her depression or confide in any of the people around her, not even her family.
The disorder haunted Zeina for years. Its effects started to take a toll on her physical health, demonstrated in severe weight loss; unwillingness to get out of bed; and general fatigue.
After experiencing these symptoms, Zeina could no longer ignore the situation. So, she turned to specialists and social therapists online when she was 25. “There were no available trustworthy psychiatrists in Syria. I could not trust the medications they prescribed, particularly those containing opioids,” said Zeina.
Zeina did not want to go to a psychiatrist, because she did not feel safe to share her feelings, ideas, or private details with strangers. Even if that sharing is with doctors specialized in treating mental disorders.
In this investigation, Enab Baladi discusses psychological treatment in Syria from a societal perspective and the priority of addressing mental disorders, especially since psychiatrists have cautioned against a “tsunami of psychological illnesses” due to curfews and home quarantine this year, enforced as a precaution against the spread of COVID-19.
Crises’ impact on mental health
Attempts to break out of the darkness of psychological turmoil
Therapy is still underway, but after several counseling sessions with online social therapists, Zeina was able to overcome the “chronic depression” she was diagnosed with a few years ago.
In UNICEF’s Mental Health and Psychological Technical Note, mental health is defined as “a condition in which each individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community,” which can be promoted through psychological support, whether external or local.

A group of Syrian men smoking cigarettes in southern Damascus – 2 February 2018 (Lens of Young Damascene)
Vulnerable groups in society are considered the most in need of the different levels of psychosocial support. These groups include children, adolescents, people with disabilities, single and providing women, survivors of torture and sexual violence, and individuals suffering from previously diagnosed mental disorders.
Since online psychotherapy is based on the interaction between two people and often takes the form of conversation, the United Nations Development Program in Syria (UNDP) launched a service program named Fadfada to provide psychosocial support to the public last August.
Fadfada, according to the managing website, is a service provided by professionals from various fields, seeking to offer psychosocial support to those under the age of 18.
UNDP posted a registration link and pledged to maintain the confidentiality of the beneficiaries’ information.
Introducing the service, the website said that difficult conditions and the impact of the daily challenges that people encounter give rise to fear, depression, shame, irritation, grief, and other feelings and states of mind, usually associated with an excessive appetite for food, lack of focus, and troubled relations with family, friends, and colleagues.
Because there is no shame in asking for help, according to the website, Fadfada is deemed a favorable space for people to narrate their suffering to psychologists and doctors, who would assist them to conquer the experiences they are going through.
Successive setbacks doubled the psychological crises
Ibrahim al-Ayed, 55 years old, fell to a state of psychological distress due to several personal crises in the past few years. He lost his public service job after a 3-month arbitrary detention in 2011; his four children were unable to pursue their education; he lost much of his savings to secure his family’s needs. Overwhelmed by all these losses, Ibrahim decided to visit a psychiatrist. However, he did not receive adequate psychological counseling because he could not afford the high costs of the procedure.
Psychological disorders result from “the individual’s inability to deal with the acute economic crisis that the country is witnessing. Hence, as soon as a person feels the loss of financial stability, mental instability emerges,” the Syrian psychologist Salwa Orabi told Enab Baldi.
The value of the Syrian pound dropped to an unprecedented level this year. The markets are also affected by these successive setbacks, which led to further price inflations and the deterioration of the already poor standards of living in areas across Syria.
Fatima, 40 years old, who requested that her last name be withheld, lives with her five children in Idlib city in northern Syria. Fatima had sporadic body aches but did not suffer from any chronic diseases. The situation being thus, an internal medicine physician, she had seen, referred her to the psychological support office at Aidoun Medical Center. The internist could tell that she was incredibly lonely and sad.
Enab Baladi contacted the center. The administration reported that Fatima felt abandoned after her children married and left her on her own. Fatima married against her family’s wishes; thus, her husband prevented her from visiting or communicating with them. She also suffered from her husband’s “temperament” that caused them to have a troubled relationship.
Fatima no longer visits her family or friends, and “has an introverted behavior and is unable to do even the simplest housework,” the center’s administration told Enab Baladi.
In an interview with Enab Baladi, mental health consultant Wael Arras attributed reported mental disorders among women, and their inclination to commit suicide in some cases, to domestic violence, which has increased during quarantine and COVID-19 outbreaks.
Domestic violence has psychological bearings on women, which includes beating, insults, confinement at home, or even threats of violence and humiliation, Arras added.
Having attended several sessions with a specialist, who provided her with a treatment program to stick to, Fatima’s condition improved by nearly 45 percent, and her life relatively returned to normal.
Poll: Treatment as an option for coping with mental disorders
In an online survey conducted by Enab Baladi , the majority of participants, 366 persons, said that they would seek treatment or psycho-social support from specialized centers should they go through experiences that lead to psychological repercussions.
Out of the total, 57 percent of the participants considered psychological treatment a priority to overcome any psychological disorder that they suffer from.
Meanwhile, 43 percent felt that psychological treatment would not be their option if they faced any difficulties or psychological troubles.
Distrust of the therapeutic relationship
One of many reasons that prevent individuals from seeking psychological counseling
Millions of Syrians are enduring the consequences of the conflict in Syria. These have bred several mental health disorders and psychosocial difficulties as a result of alarmingly rising rates of conflict-related violence and levels of anxiety. This is in addition to day-to-day pressures of displacement, poverty and lack of basic needs and services, as well as the constant risks of violence and exploitation, isolation, discrimination, loss of family and community support, and uncertainty about the future.
Syrians are overcome by the presiding sentiments of loss and grief, whether the loss of deceased family members, relations, or property and possessions. Missing family protection causes great psychological strain. Internally displaced Syrians and refugees abroad often hope for good news about their loved ones, but all they get is confusing information and uncertainty, as in the case of detainees or forcibly disappeared relatives or friends.
Victims of these psychosocial disorders are mostly children, particularly since more than two million children have been forced to flee their homes and face the trauma of displacement inside Syria, while nearly a million others have been coerced to immigrate.
One of the principal reasons that prevent Syrians from seeking psychological counseling at specialized centers is poor living standards. This particularly applies to 2020 with the U.S. sanctions that affected the Syrian pound and the standing of the middle class, which lost a lot of its capital and children, who immigrated and sought refuge in Arab and Western countries. Class disparity occurred as well, with the middle class pressed into the ranks of the impoverished.
Psychosocial support is a natural need for everyone, but the culture of psychotherapy is absent in the Syrian society. This is because people believe that it is specific to people with severe mental illnesses, but there is no dividing line between psychological disorders and mental illnesses which affect each other.
Psychotherapy is a part of the individual’s life and covers all his/her needs in terms of assistance; financial, medical, moral, or otherwise.
Due to our cultural upbringing, we tend to view a person who turns to a psychiatrist as a crazy person, which is not true. Society stigmatizes patients and their families. People, however, must understand the reality of the crises they are going through rather than deny it, be it physical or psychological.
Another reason why some individuals refuse to seek psychiatrists, even if they are aware of the importance of psychotherapy or are financially able to do so, is that they lack confidence in the patient-therapist relationship. This reason might as well be valid in the case of the psychologically troubled individual who lives daily in psychological treatment support centers.
To help patients out of their psychological crisis, which is the goal of every psychological treatment, the therapists’ relationship with patients must be based on trust, loyalty, and reassurance. These sentiments are a priority to create a positive interaction. When they decide to start psychological counseling, patients tend to believe that psychiatrists are the last resort to save their lives.
Syrian society’s false beliefs that stigmatize mental health
Syrian society’s false beliefs that stigmatize mental health
The social perception in Syria about mental illness was developed by society itself, the psychiatrist at Ghazi Center for Mental Health in Turkey, Jalal Nofal, told Enab Baladi. There are misconceptions about psychiatry that are not limited to a specific group within the Syrian society and are affected by a misinterpretation of religion and other false beliefs.
“Many people believe that psychological problems are related to a weakness in personality or faith. Therefore, they resort to social figures that share their beliefs. They might appeal to religious personalities when the problem is seen as related to faith,” Nofal said.
Nofal added that fragile people refer to their social circles for advice, which might turn to be harmful, for it happens that they hear labels as “you have a weak personality! You must be stronger and better.” These people, who are part of society, internalize these claims subconsciously that end up stopping them from seeking psychotherapy.
The decline in education; social fragmentation, and lack of rational understanding in Syria, as well as the decrease in the number of health institutions and the quality of the services they provide, have all led people to resort to their familiar local resources (religion scholars, superstitions, and persons or entities claiming specialization in psychotherapy), which offer them faulty concepts and methods and have a negative influence on any subsequent treatment efforts, Nofel added.
“War has shattered the society’s rational frameworks, the reason why people started to resort to irrational methods of treatment,” according to Nofal. The exact proportions of the related-situation in Syria cannot be fathomed in the meantime because the Syrian society is in a state of conflict that had devastating impact on mental health and local health resources (healthcare sector). However, any attempts to measure the extent of psychological problems in Syria will show that they outweigh the available healthcare resources.
In connected and cohesive societies, people exchange their best experiences and come up with solutions to afford a positive environment and healthcare resources and shelters, according to Nofal.
As a result of absent mental health culture,
psychiatric services in northwestern Syria are ineffective
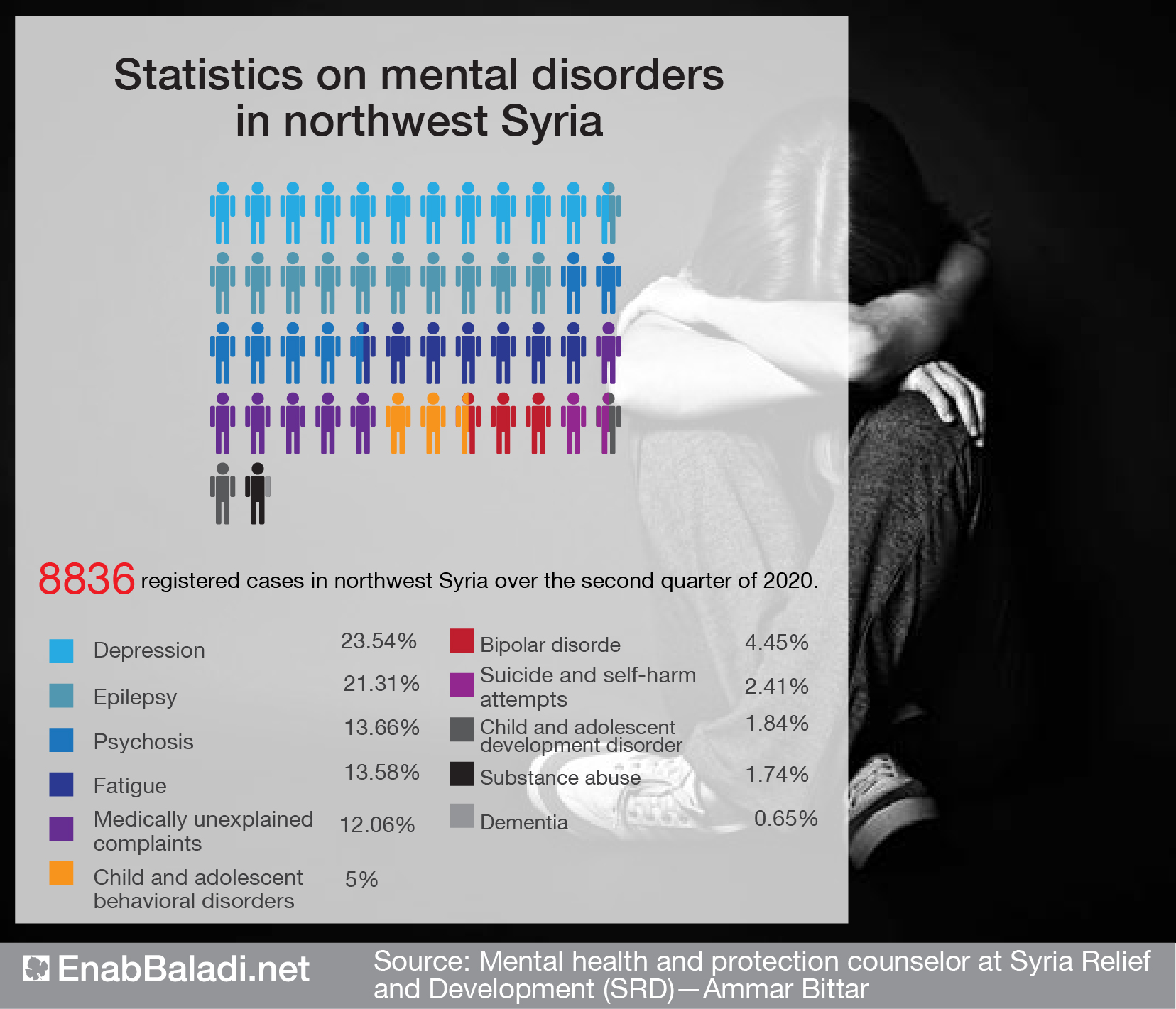
Areas outside the Syrian regime’s control in northwestern Syria suffer from poor medical services, which fail to respond to psychosocial crises, Samer Assayed Ali, officer in charge of the psychological support programs at the Syrian American Medical Society (SAMS), foundation operating in northern Syria, told Enab Baladi. “There are only two psychiatrists in northwestern Syria. They work in Sarmada and Azaz mental health centers, providing specialized counseling for severe and mild cases.”
The organizations concerned with psychosocial support in northwestern Syria make available such services through recruiting psychosocial support specialists. These staffers are trained to conduct one-on-one and group support sessions, in addition to raising awareness on mental health issues, according to Ali.
SAMS psychological support specialists are trained on the developed problem management approach (PM+) by the World Health Organization (WHO), on suicide prevention, and on addressing postpartum depression through programs conducted in cooperation between the WHO, mental health technical groups, and local organizations, Ali added.
The foundation is designing an educational curriculum for psychosocial support workers to be complete within the six upcoming months, according to Ali. It will also train 30 local women on an advanced approach—Common elements treatment approach—in cooperation with the British John Hopkins University. This training program will continue for two years.
The shortage of psychiatrists in northern Syria has prompted the WHO, in cooperation with its partner local organizations, to train doctors on mental health Gap Action Programme (mhGAP) which qualifies non-specialist doctors to provide psychological treatment to mild cases and address most common disorders.
To SAMS, the lack of psychiatrists and psychotherapists trained to provide non-pharmacological psychotherapy is one major challenge, given that non-drug therapy is the biggest gap in mental health services that need to be greatly developed, said Ali.
“The union’s work was particularly difficult due to lacking crisis-related expertise, in addition to the absence of a culture that advocates mental health in the Syrian society before the revolution,” Bishr Hajj Hussein, psychotherapist and mental health coordinator at the Union of Medical Care and Relief Organizations (UOSSM), operating in northwestern Syria, told Enab Baladi.
According to Hajj Hussein, mental health is associated with mental illness and hence with mental institutions exclusively. Therefore, people did not respond to psychological support in the past and concerned departments did not have an effective role.
Over time, psychological responses became organized as they adhered to international standards; the role of involved workers became more defined, and organizations started to have an actual influence on the Syrian society.
Various services
UOSSM provides psychological treatment to cases ranging from severe, which require hospitalization and temporary stay in hospital, to more moderate ones, according to Hajj Hussein.
In addition, the union offers psychological counseling services over the phone by a specialized team of eight workers. They cover most of the region’s areas to facilitate the service’s access to homes during the pandemic. The calls are “secured communications and are governed by approved global standards,” said Hajj Hussein.
The union also provides mental health services which are integrated into the programs of its primary health care clinics (dispensaries). There are 17 such clinics in northern Syria, operated by general medicine practitioners trained in psychological responses, and health workers, who attend to the cases that seek the clinics.
UOSSM runs a mobile clinic as well, managed by general medicine practitioners trained on psychological interventions based on WHO programs, in cooperation with health workers specialized in psychological counseling.
Ongoing challenges and concerns
UOSSM is mostly concerned over funding cuts, which might hamper the services offered to the affected people, according to Hajj Hussein.
The social stigma developed against seeking psychological treatment, even though people recognize their need for such specialized responses, poses a constant challenge for health workers. This stems from the stereotypes associated with psychological treatment. But the repercussions of the conflict and the fear it instilled among people of losing their relatives or displacement from their areas of origin have affected these attitudes and, most importantly, revealed the people’s need for periodic psychotherapy sessions.
Psychosocial response within affected local communities starts voluntarily and spontaneously, Qutaiba al-Khalil, a consultant for safe programming and protection at the American Chemonics Foundation, concerned with supporting medical projects, told Enab Baladi. The communities’ reaction precedes the action put by humanitarian organizations, and it is usually guided by dignitaries, families themselves, the network of social relations, and the communities positive customs and traditions.
For their part, organizations should advance further support to local communities, according to al-Khalil, so that the response is directed towards the psychosocial difficulties and challenges arising as a result of their predicaments.
Organizations tend to start with an assessments of the communities general needs, including psychosocial ones, and the necessary specialized psychological services, particularly when traditional services stop being operative during disasters.
The organizations’ preliminary role is then manifested in rehabilitating workplaces; providing logistic support for activities, and recruiting and qualifying local cadres who can implement programs appropriate to the context and the specific needs of each community.
There is a major challenge to psychological support activities designed to respond to a variety of emergencies, including those applied in Syria, according to al-Khalil. These are related to the content and model of these activities, which are often structured by knowledgeable and renowned personalities. These designers have mastered the technical dimension of the process, but still they may not be familiar with local sensitivities towards raising some issues, such as those discussed during consultations. This gap could discourage individuals from seeking psychosocial treatment.
Local employees also contribute to this challenge, as they treat activity structures and content as fixed texts that cannot be modified and that should be applied strictly. This attitudes result in the inadequacy of the activities; their failure to meet the assessed needs; and the potential aversion that beneficiary tend to express.
Opting for unfamiliar activities; using incomprehensible terms, at times, showing disregard for gender sensitivity or the local culture, in the contents of some of the psychological support activities, constitute a barrier to a large segment of the beneficiaries, who turn away from these activities. Sometimes it is the organizations’ failure to demonstrate, in tangible ways, the outcome of these activities for local communities that makes such activates appear as of little or no use.
According to al-Khalil, the best way to draw the attention of local communities to the importance of these activities and to gain their confidence perhaps lies in ensuring that these activities are connected with and integrated into other response sectors, such as education, health, shelter, etc., and ensuring that they are carried out by the local community—i.e. interventions should be designed and implemented by a local staff based on international standards. Therefore, the concerned organizations must seriously consider the mechanisms that may already exist in the community before providing psychosocial support.
Government neglect before 2011:
No one is concerned about the psychological wellbeing of Syrians
“Before the Syrian revolution, mental health services were limited to Inpatient treatment. Furthermore, only persons with chronic disorders were offered these services,” dr. Ahmed Sheikhani from ReliefWeb organization, operating in northern Syria, told Enab Baladi. This reinforced the Syrian society’s lack of interest in mental health.
Only a few state-run hospitals provided specialized mental health services, such as Ibn Sina hospital for psychiatric diseases in Damascus and Ibn Khaldun hospital in Aleppo. Aside from these, mental health was addressed by secondary departments in some hospitals, such as Mouwasat hospital.
In 2004, a private mental health hospital was established in Harasta, Damascus countryside.
Enab Baladi tried to communicate with the Syrian Red Crescent (SRC) in Damascus, but it received no response so far.
With the arrival of Iraqi refugees to Syria in 2007, medical centers, under the auspices of the United Nations, started operating multidisciplinary clinics, encompassing a psychiatrist, a psychotherapist, and a social worker. These were founded to provide consultations to Iraqi families exclusively.
After 2011, in the areas controlled by the Syrian regime and those held by the opposition in northern Syria, these services stopped. This is when NGOs began to provide psychosocial support services to compensate for the shortcomings of government centers in general, according to dr. Sheikhani.
These organizations provide only psychosocial support services because curative support cannot be offered as the conflict continues.
These services are provided by community centers that organize protection-related and psychological support activities aimed at children and women. However, these centers are not specialized.
Community centers are thus often annexed to primary health centers that provide medical services in general. According to dr. Sheikhani, this merger resulted in training general practitioners on the methodology and guides addressing some mental disorders. Aided by these training programs, doctors were able to diagnose and manage cases.
if you think the article contain wrong information or you have additional details Send Correction
النسخة العربية من المقال
-
Follow us :
Most viewed
- Turkey moves to deploy air defense system in Syria
- Intentions for popular resistance amid Israeli escalation in southern Syria
- SDF to withdraw from Aleppo neighborhoods following agreement with Damascus
- Washington's conditions raise questions about its openness and goals in Syria
- Al-Sharaa names new Syrian government












 A Syrian refugee girl in Gaziantep, southern Turkey - 12 September 2015 (Afeinkolik Shutterstock)
A Syrian refugee girl in Gaziantep, southern Turkey - 12 September 2015 (Afeinkolik Shutterstock)





 A
A
A
A
A
A











 More In-Depth
More In-Depth